NAHAM AccessKeys® Defined: What Should I Measure?

As the old adage goes, “you cannot manage what you cannot measure,” and NAHAM knew this well when the nationally recognized NAHAM AccessKeys were first introduced. Today, as we prepare for the introduction of a new AccessKey, benchmarking financial clearance, it’s more important than ever to remember and discuss the KPIs and metrics that matter most to Patient Access. As a leader and veteran of the Revenue Cycle and more specifically, Patient Access, it is my pleasure and honor to contribute NAHAM AccessKeys Defined: What Should I Measure? to the latest publication of NAHAM’s Access Management Journal, the official quarterly publication of patient access news and insights. As AccuReg’s VP of implementation and with more than ten years of experience serving as a senior leader in Patient Access, I am most passionate about bringing awareness, best practices, and continued education to the NAHAM and healthcare community about the supreme importance of a well-functioning and efficient front-end patient access department and the NAHAM AccessKeys.
Read the original article here.
Patient Access teams serve a unique role in the revenue cycle. Team members have a responsibility to ensure clean claims and a positive first contact experience with the patient and their families. With reimbursement models not only using traditional billing methodologies, payers, including CMS, are expanding to include clinical outcomes and patient satisfaction as incentives for higher levels of reimbursement. Patient Access teams contribute to positive financial and clinical experiences through strong registration processes that are repeatable and dependable.
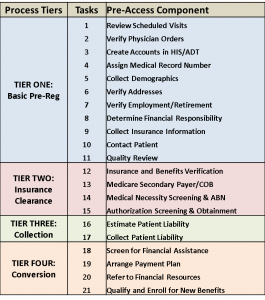 There are two existing NAHAM AccessKeys® related to the pre-registration process, and a new key soon to be introduced for financial clearance. Pre-registration of patients is a must for hospital systems attempting to financially clear their scheduled patients prior to service. Those systems meeting the best practice standards have implemented clear policies and processes for teams and provided them with tools for success. These metrics require an understanding of pre-registration process tiers. The higher the level of understanding and policy adherence, the higher the opportunity to financially clear a patient prior to arrival and streamline their check-in process.
There are two existing NAHAM AccessKeys® related to the pre-registration process, and a new key soon to be introduced for financial clearance. Pre-registration of patients is a must for hospital systems attempting to financially clear their scheduled patients prior to service. Those systems meeting the best practice standards have implemented clear policies and processes for teams and provided them with tools for success. These metrics require an understanding of pre-registration process tiers. The higher the level of understanding and policy adherence, the higher the opportunity to financially clear a patient prior to arrival and streamline their check-in process.
NAHAM AccessKeys® P-3 is the most basic key and the most easily managed from a reporting standpoint.
This metric includes all pre-registrations initiated or started for the period specified for procedures scheduled within 48 hours of arrival. This calculation traditionally does not include reference labs, add-on or walk-in patients or accounts scheduled on a Friday for Monday service if the pre-service team is not scheduled to work weekends. This would be the same for any account scheduled on a Saturday or Sunday for a Monday or Tuesday procedure. This calculation could include the account if pre-registration was completed at any tier within 48 hours in both the numerator and denominator, to reflect staff work effort.
Because this metric measures the percentage of scheduled patients where pre-registration processes were initiated but not necessarily completed, this KPI is an activity measure, not an outcomes measure. To fully assess the performance of a pre-registration team, P-3 pre-registration rate should be used in conjunction with P-4 pre-registration completion rate. For example, a 90% pre-registration rate appears to indicate high performance. However, if the same hospital’s completion rate is 30%, it is unlikely they are achieving the positive outcomes they desire. A hospital with an 80% pre-registration rate and 80% pre-registration completion rate likely sees greater benefits to the revenue cycle and to patient experience. See NAHAM’s pre-registration process tiers for more information and to assess your facility. Achieving a level four in the tier structure would be optimal performance.
The base data for this metric is an expanded set of data from the same dataset used to determine P-3 pre-registration rate. The number of pre-registrations are encounters that meet the minimum standard of a tier one. s – 11 tasks should be completed before including the account in this figure.
This KPI requires a pre-registration workflow and reporting system that interfaces with scheduling and/or ADT systems. It is difficult to track task-level completion of pre-registered accounts and then report using manual methods. Therefore, NAHAM recommends looking to automated reporting systems to track and report pre-registration completion rates. Tracking completion rate of pre-registered accounts supports a positive patient experience by:
- Identifying the pre-registered patients at time of arrival for to fast-track
- Confirming which tasks were completed so the patient is not asked the same questions
- Confirming tasks not completed so all processes can be completed at registration
- Allowing the pre-registration team to communicate special information about the patient to the arrival team such as the need for a wheelchair, a language interpreter, vision or hearing impairment or other special handling instructions such as fear of a procedure.
Results should be reported in a manner that quantifies the level of the pre-registration, thus reflecting pre-registration process impact on the full revenue cycle. . This information also assists Patient Access leaders understand areas of improvement and identify barriers to achieving tier four pre-registration and financial clearance.
Financially-Cleared Patients
NAHAM is introducing a new key in 2019 to define financially-cleared patients. The core definition for financial clearance includes the number of patient encounters with clear payment paths resulting in a zero balance at account adjudication. Financial clearance can be achieved through POS collections, payment plan offerings, referral and acceptance to financial assistance, referral and acceptance to other financial institutions and/or referral and acceptance to government assistance programs.
Reaching full financial clearance, including tier four pre-registration, would be an indicator of mature processes in Patient Access relating to patient financial communications. Leading practice also means initiating the financial conversation early in the pre-registration process for scheduled visits and having the tools and training for frontline registration staff, including emergency room staff, to successfully collect from patients or refer them down the proper financial pathway at time of registration for non-scheduled patients. Tracking mechanisms must be built within the core ADT or third-party systems for ease of reporting.
Technology should be optimized and adopted by staff and is necessary to achieve “best” level results. Patient Access leaders need a mechanism to ensure tool and process adoption, which should include staff scorecards that reflect other NAHAM AccessKeys® and hold staff accountable.
As reimbursement becomes more complex, patients solidify their roles as consumers and expectations for streamlined processes in access to care fosters competition, leading to patient care choices. It is imperative that access teams meet increasing demands to keep financial solvency for their hospital systems. Using metrics to track performance and ease of reporting abilities empowers leaders and their teams to be successful.
Melissa Salyer is the vice president of implementation at AccuReg. She has over 10 years of Patient Access senior leadership in a hospital setting and has been a member of award-winning revenue cycle teams since 2003. She is an active member of NAHAM and HFMA. She is HFMA CRCR certified and a Six Sigma Yellow Belt. She was a founding member of the NAHAM Industry Standards Committee.